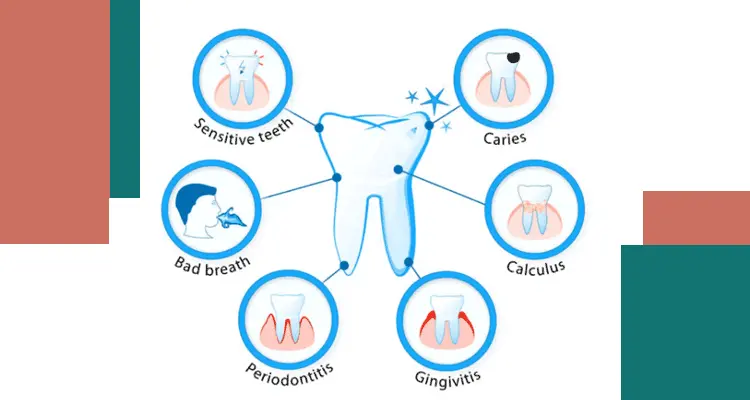
Dental diseases encompass a spectrum of conditions affecting the teeth, gums, and supporting structures of the mouth. These can range from minor nuisances like bad breath to severe complications like tooth loss and even infection.
The good news is that many dental diseases are largely preventable with a consistent oral hygiene routine and regular dental checkups. From tooth decay and gum disease to lesser-known conditions like hyperdontia, here we explained the causes, symptoms, and treatment options for each.
1. Tooth Decay (Dental Caries)

Tooth decay, often referred to as cavities, is the most prevalent dental disease. It occurs when plaque, a sticky film of bacteria, builds up on the surface of the teeth.
The bacteria feed on sugars in food and drinks, producing acids that erode tooth enamel, the hard outer layer of your teeth. Over time, this erosion can lead to cavities or holes in your teeth.
Symptoms of tooth decay may include:
- Toothache, especially when eating or drinking something sweet, hot, or cold
- Sensitivity in the teeth
- Visible holes or pits in the teeth
- Stained teeth (brown, black, or yellow)
To prevent tooth decay, practice good oral hygiene by brushing your teeth twice a day with fluoride toothpaste and flossing daily. Regular dental checkups and cleanings are also crucial for early detection and treatment of cavities.
2. Gum Disease (Periodontal Disease)
Gum disease is an inflammation of the gums caused by plaque buildup. If left untreated, it can progress to periodontitis, a severe gum infection that damages the soft tissue and bone that support your teeth. This can lead to tooth loss.

Symptoms of gum disease can include:
- Red, swollen, or tender gums
- Bleeding gums when brushing or flossing
- Loose teeth
- Receding gums (gums that pull away from the teeth)
- Bad breath (halitosis)
Maintaining good oral hygiene is essential for preventing gum disease. Brushing, flossing, and regular dental cleanings help remove plaque and keep your gums healthy. In some cases, your dentist may recommend additional treatments for gum disease.
3. Sensitive Teeth
Tooth sensitivity occurs when the dentin, a layer beneath the enamel, becomes exposed. Dentin contains tiny tubules that lead directly to the nerves in the tooth. When these tubules are exposed to hot, cold, sweet, or acidic foods and drinks, they can trigger a brief, sharp pain in the tooth.
Causes of sensitive teeth can include:
- Worn tooth enamel due to brushing too hard or using abrasive toothpaste
- Gum recession
- Cracked or chipped teeth
- Worn-down fillings
There are various desensitizing toothpastes and mouthwashes available to help manage tooth sensitivity. Your dentist can also recommend other treatment options depending on the cause of your sensitivity.
4. Cracked or Broken Teeth

Cracked or broken teeth can happen due to various reasons, such as biting down on hard objects, injury, or teeth grinding. The severity of the damage determines the symptoms you experience. A small crack may not cause any pain, while a larger crack or break can lead to significant pain, sensitivity, and even toothache.
If you suspect a cracked or broken tooth, it’s crucial to see your dentist as soon as possible. Early diagnosis and treatment can help prevent further damage and potential tooth loss. Depending on the extent of the crack or break, treatment options may include fillings, crowns, or root canals.
5. Receding Gums
Receding gums occur when the gum tissue around your teeth starts to shrink or pull away, exposing more of the tooth root. This can be caused by poor oral hygiene, gum disease, hormonal changes, or aggressive brushing. Receding gums can make your teeth look longer and increase your risk of tooth decay and sensitivity.
Early intervention is crucial to prevent further gum recession and potential tooth loss. Your dentist can recommend treatment options based on the severity of the receding gums. This may include professional cleaning, deep cleaning (scaling and root planing), or gum grafting procedures.
6. Root Infection

A root infection, also known as an abscessed tooth, occurs when bacteria reach the inner pulp of the tooth, which contains nerves and blood vessels. This infection can cause significant pain, swelling, and sensitivity.
Symptoms of a root infection may include:
- Throbbing toothache that worsens at night
- Sensitivity to hot and cold temperatures
- Swollen gums
- Pus around the tooth
- Swollen lymph nodes in the face or neck
- Fever
Root infections are a dental emergency and require immediate treatment. Your dentist will likely prescribe antibiotics to fight the infection and may perform a root canal to remove the infected pulp and save the tooth. In some cases, the tooth may need to be extracted.
7. Enamel Erosion
Enamel erosion is the gradual loss of the tooth’s hard outer layer, enamel. Unlike cavities caused by bacteria, enamel erosion is caused by acidic foods and drinks, as well as frequent brushing with abrasive toothpaste or brushing too hard. Erosion can lead to sensitive teeth, discoloration, and increased risk of cavities.

Here are some signs of enamel erosion:
- Increased tooth sensitivity
- Transparent or thin-looking teeth
- Rounded edges of the teeth
- Discoloration (teeth may appear yellow)
To prevent enamel erosion, limit your intake of acidic foods and drinks. Brushing with a soft-bristled toothbrush and using a fluoride toothpaste can also help protect your enamel.
Dentist can recommend you specific strategies to prevent further erosion and may suggest treatments like fluoride treatments or bonding to restore tooth structure.
8. Dry Mouth
Dry mouth, a condition where your mouth doesn’t produce enough saliva, can be caused by various factors, including medications, certain medical conditions, and aging.
Saliva plays a vital role in maintaining oral health by washing away food particles, neutralizing acids produced by bacteria, and preventing infections.
Symptoms of dry mouth may include:
- A dry, sticky feeling in the mouth
- Difficulty speaking or swallowing
- A dry, cracked tongue
- Bad breath (halitosis)
- Increased risk of cavities
If you experience symptoms of dry mouth, consult your doctor or dentist to determine the underlying cause and discuss treatment options. Staying hydrated by drinking plenty of water throughout the day can help alleviate dryness. Your dentist or doctor may also recommend sugar-free lozenges, artificial saliva products, or medications to stimulate saliva production.
9. Teeth Grinding (Bruxism)
Teeth grinding, medically known as bruxism, is a condition where you unconsciously grind or clench your teeth. It can happen during sleep (sleep bruxism) or while awake (awake bruxism).
Bruxism can cause various dental problems, including:
- Worn down teeth
- Increased tooth sensitivity
- Jaw pain
- Headaches
The exact cause of bruxism is unknown, but stress, anxiety, and certain medical conditions may contribute to it. Treatment options for bruxism may include wearing a mouthguard at night to protect your teeth, relaxation techniques to manage stress, and addressing any underlying medical conditions.
10. Wisdom Teeth Problems

Wisdom teeth are the four permanent adult teeth located at the very back of your mouth, usually erupting between the ages of 17 and 25. There isn’t always enough space in the jaw for wisdom teeth to erupt properly.
This can lead to impaction, where the wisdom tooth gets stuck under the gum or bone. Impacted wisdom teeth can cause pain, swelling, infection, and damage to surrounding teeth.
In most cases, impacted wisdom teeth need to be extracted by an oral surgeon to prevent future complications. Your dentist will take X-rays to assess the position of your wisdom teeth and recommend the best course of action.
11. Oral Cancer
Cancers that develop in the lip, mouth, tongue, throat, and other parts of the oral cavity fall under the umbrella term of oral cancer. Tobacco use (including chewing tobacco), excessive alcohol consumption, and human papillomavirus (HPV) infection are major risk factors for oral cancer.

Early signs and symptoms of oral cancer can include painless mouth sores, lumps in the mouth or neck, white or red patches on the gums or tongue, unexplained bleeding in the mouth, and difficulty swallowing or chewing.
Regular dental checkups are crucial for early detection of oral cancer, as treatment success rates are significantly higher when the disease is caught in its early stages.
12. Oro-dental Trauma
Injuries to the teeth, jaw, and surrounding tissues are classified as oro-dental trauma. This can happen due to accidents, falls, contact sports injuries, violence, or even improper use of dental tools.
The severity of oro-dental trauma can vary greatly, ranging from chipped or cracked teeth to complete tooth avulsion (tooth being knocked out). Prompt dental attention is crucial for treating oro-dental trauma to prevent complications like infection, nerve damage, or tooth loss.
Depending on the extent of the injury, treatment options may include splinting (stabilizing loose teeth), root canal therapy (for injuries affecting the tooth pulp), or dental implants (to replace missing teeth).
13. Noma (Gangrenous Stomatitis)
This is a rare but devastating infectious disease that primarily affects children living in poverty with poor oral hygiene and malnutrition.
Caused by a combination of bacterial infections, noma starts as a small sore on the gums and rapidly progresses, causing gangrene (tissue death) and destruction of facial tissues.
Early intervention with antibiotics, improved nutrition, and supportive care are essential to stop the progression of noma and prevent potentially fatal complications.
14. Cleft Lip and Palate
These are birth defects that occur when the structures of the upper lip or roof of the mouth (palate) don’t fuse together properly during fetal development. The severity of cleft lip and palate can vary, and it can affect a child’s appearance, ability to eat and speak, and even cause hearing problems.
Fortunately, cleft lip and palate can be effectively treated with surgery, often performed in stages throughout childhood. Speech therapy and other interventions may also be necessary to help children with cleft lip and palate develop normal speech patterns.
15. Spacing Between Teeth: Addressing the Gap
Gaps between the front teeth, medically known as diastema, are a common dental concern. While some people embrace the diastema gap as a unique feature, others may seek to close it for aesthetic reasons. There are several causes for gaps between teeth, including:

- Small jaw size: Sometimes, the jaw simply doesn’t have enough space to accommodate all the teeth comfortably, leading to gaps.
- Missing teeth: If a baby tooth falls out prematurely, the adult tooth may erupt in an unexpected position, creating a gap.
- Tongue thrusting: Persistent habits like tongue thrusting can push teeth forward, causing gaps to develop.
- Genetics: Hereditary factors can influence jaw size and tooth development, potentially leading to gaps.
Several orthodontic options can address gaps between teeth, depending on the severity and your desired outcome. Braces are a traditional method that uses gentle, continuous pressure to move teeth into their ideal positions.
Clear aligners offer a more discreet alternative for mild to moderate gaps. In some cases, dental bonding or veneers can be used to close small gaps cosmetically. Consulting with an orthodontist can help determine the best approach for your specific situation.
16. Too Many Teeth: Hyperdontia Explained
Hyperdontia refers to a rare dental condition where a person has extra teeth beyond the typical 20 baby teeth and 32 permanent adult teeth. These extra teeth can erupt anywhere in the mouth, but they most commonly appear behind the front incisors or wisdom teeth.
The exact cause of hyperdontia is unknown, but genetics may play a role. Extra teeth can sometimes impact surrounding teeth, causing misalignment or crowding.
In such cases, your dentist or orthodontist may recommend removing the extra teeth and potentially using braces to realign the remaining teeth. Early detection and treatment of hyperdontia can help prevent future complications and ensure optimal oral health.
17. Yellow Teeth
Yellowing teeth are often a natural consequence of aging. As the outer layer of enamel thins over time, the yellowish dentin underneath becomes more visible.
Certain lifestyle choices like smoking, excessive coffee or tea consumption, and frequent use of chromogenic (staining) foods like berries or curries can also contribute to yellowing. In many cases, maintaining good oral hygiene with regular brushing and flossing can help manage yellowing.
Professional teeth whitening treatments offered by dentists can significantly brighten yellowed teeth. However, it’s important to understand that whitening treatments may not address the underlying cause and yellowing can recur over time.
18. Stained Teeth
Stains are typically caused by external factors that discolor the tooth’s surface enamel. Common culprits include chromogenic foods and drinks, tobacco use, and certain medications. Poor oral hygiene can also contribute to stains by allowing plaque to build up and harbor stain-causing substances.
The approach to removing stains depends on the severity and cause. Professional cleaning by a dentist can effectively remove most surface stains. For stubborn stains, your dentist may recommend stronger whitening treatments or cosmetic procedures like veneers.
19. Toothache
Toothache is a symptom, not a disease itself, and can indicate various underlying dental problems.
Here’s how it relates to yellow and stained teeth:
While yellowing teeth don’t directly cause toothaches, the underlying causes of yellowing, like gum disease or tooth decay, can lead to pain and discomfort. Similar to yellow teeth, stained teeth themselves don’t cause toothaches. However, the culprits behind stained teeth, such as cavities or gum disease, can be the source of the pain.
20. Bad Breath
Bad breath, also known as halitosis, can be a source of embarrassment. While occasional bad breath might be due to strong foods, persistent halitosis often stems from poor oral hygiene or underlying dental issues.
Here are some dental diseases that can contribute to bad breath:
- Gum Disease: Bacteria build-up at the gum line can cause inflammation and bleeding, leading to a foul odor.
- Tooth Decay: Food particles trapped in cavities can decompose and release unpleasant odors.
- Dry Mouth: Reduced saliva flow allows bacteria to thrive, creating a breeding ground for bad breath.
- Tongue Coating: Bacteria on the tongue’s surface can produce a film that contributes to bad breath.
Brushing twice daily, flossing regularly, and keeping your tongue clean are crucial for good oral hygiene and fresh breath. Regular dental checkups allow dentists to detect and address underlying issues like gum disease or cavities that might cause halitosis. If you suspect a dental problem, consult your dentist for proper diagnosis and treatment.
21. Dental Anxiety and Phobia
Anxiety or phobia can deter individuals from seeking necessary dental care. Many dental practices offer compassionate environments and techniques to manage anxiety, ensuring a comfortable and positive experience.
Dr. Md. Mostafizur Rahman Khandaker: Your Partner in Comprehensive Oral Health
Maintaining a healthy smile requires proactive care. Mostafizur’s Dental offers a comprehensive approach to dentistry, addressing conditions like cavities, gum disease, and toothaches. We also provide cosmetic solutions and treatments for anxiety. Schedule an appointment today and let our team help you achieve optimal oral health!